- Introduction
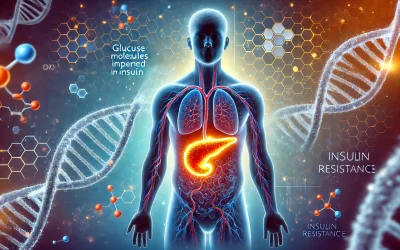
- Overview of diabetes and its systemic effects
- Defining foam/bubbles in urine
- Why changes in urine appearance matter
- Causes of Foamy Urine in Diabetic Patients
- Proteinuria and its link to kidney damage
- Diabetic nephropathy: How diabetes affects the kidneys
- Other potential contributors (e.g., dehydration, infections)
- Dietary Factors and Misconceptions
- Examining the myth: Too much protein causing foamy urine
- The role of balanced protein intake in diabetes management
- Current dietary guidelines for diabetic patients
- Beyond Protein: Other Organ Involvement
- The liver’s role in overall metabolic health
- Distinguishing kidney issues from other systemic factors
- Interplay between multiple organ systems in diabetes
- Diagnosis and Medical Management
- Diagnostic tests for proteinuria and kidney function
- When to seek professional medical advice
- Emerging diagnostic techniques and technologies
- Forward-Thinking Approaches and Future Perspectives
- Innovative research in diabetic kidney disease
- Integrative therapies: Combining lifestyle, diet, and medicine
- The future of early detection and proactive management
- Conclusion
- Key takeaways for patients and caregivers
- The importance of early intervention and continuous monitoring
- A proactive and informed approach to managing diabetes
Introduction
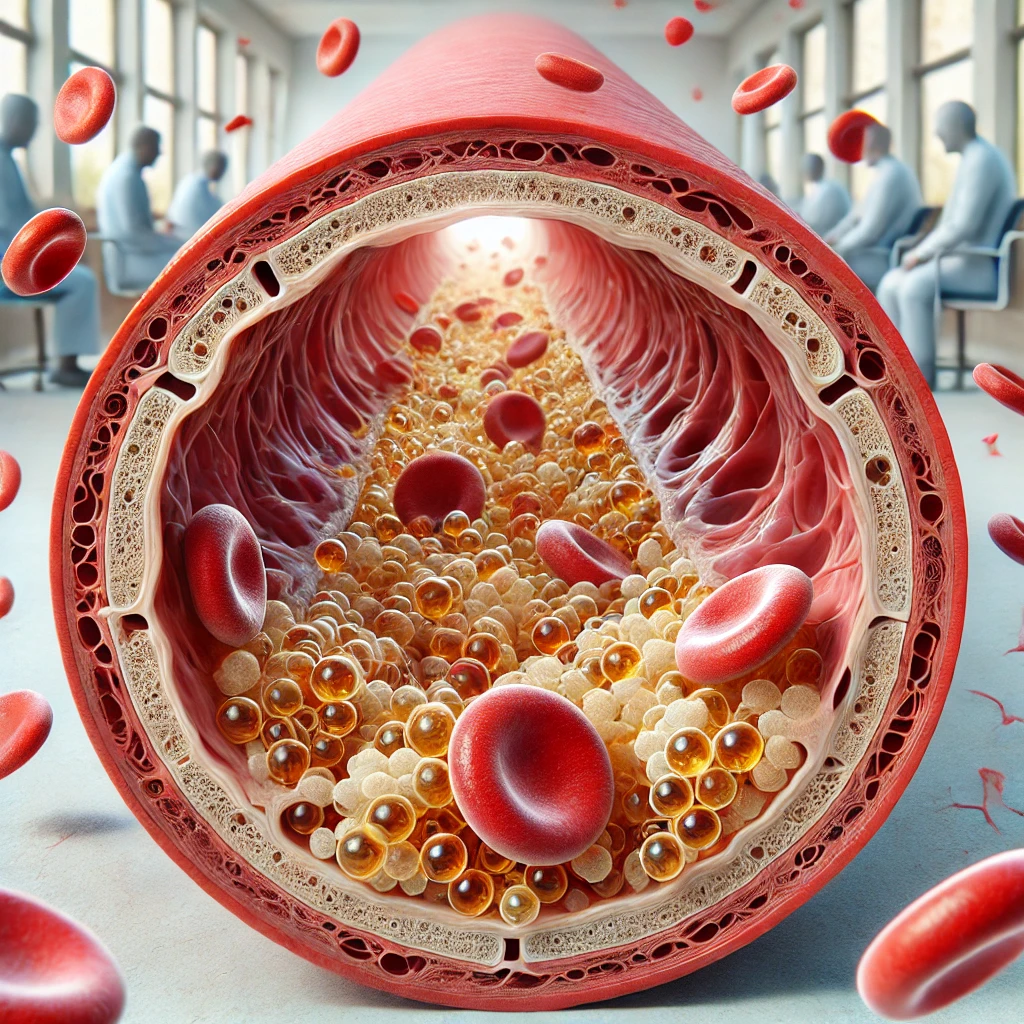
Diabetes is a complex metabolic disorder that affects multiple body systems, often leading to a range of complications that extend beyond blood sugar levels. One early and sometimes overlooked sign is the presence of foam or bubbles in the urine. This phenomenon, while potentially alarming, can serve as an early indicator of underlying kidney issues—specifically, protein leakage known as proteinuria, which is a common complication in diabetic patients.
Foamy urine occurs when proteins, which are normally retained in the bloodstream, leak into the urine due to a compromised filtering system in the kidneys. This leakage can be a signal that the kidneys are under stress or beginning to fail, especially in the context of diabetic nephropathy. Although some individuals may mistakenly attribute this condition to a high-protein diet, current evidence suggests that the cause is more intricately linked to kidney damage rather than dietary protein overload.
Moreover, while the liver plays a critical role in overall metabolic health, its direct connection to foamy urine is less straightforward. Instead, the appearance of foam in urine is most directly related to the health of the kidneys, making it a crucial symptom for early diagnosis and proactive management in diabetic patients.
This article will delve into the causes behind foamy urine, explore common misconceptions about dietary protein, and discuss the importance of early detection and innovative management strategies for kidney complications associated with diabetes.
Causes of Foamy Urine in Diabetic Patients
One of the primary reasons for foamy urine in diabetic individuals is proteinuria, which refers to the presence of an abnormal amount of protein in the urine. Under normal circumstances, healthy kidneys efficiently filter waste while retaining essential proteins in the bloodstream. However, in diabetic patients, prolonged high blood sugar levels can damage the delicate filtering units of the kidneys—the glomeruli. This damage, often referred to as diabetic nephropathy, compromises the kidney’s filtering ability, allowing proteins to leak into the urine. The resulting proteinuria is not only a sign of kidney stress but also a key early indicator of potential renal complications in diabetes.
While proteinuria is the most direct cause of foamy urine, there are other contributing factors that should not be overlooked. For instance, dehydration can concentrate the urine, making any present proteins appear more foamy. Additionally, urinary tract infections or other temporary conditions may also cause transient foaminess. However, in the context of diabetes, persistent foamy urine is more concerning as it directly points to kidney damage rather than a short-term dietary or hydration issue. Recognizing this symptom early is critical, as it allows for prompt medical intervention and can help in mitigating further renal impairment.

Dietary Factors and Misconceptions
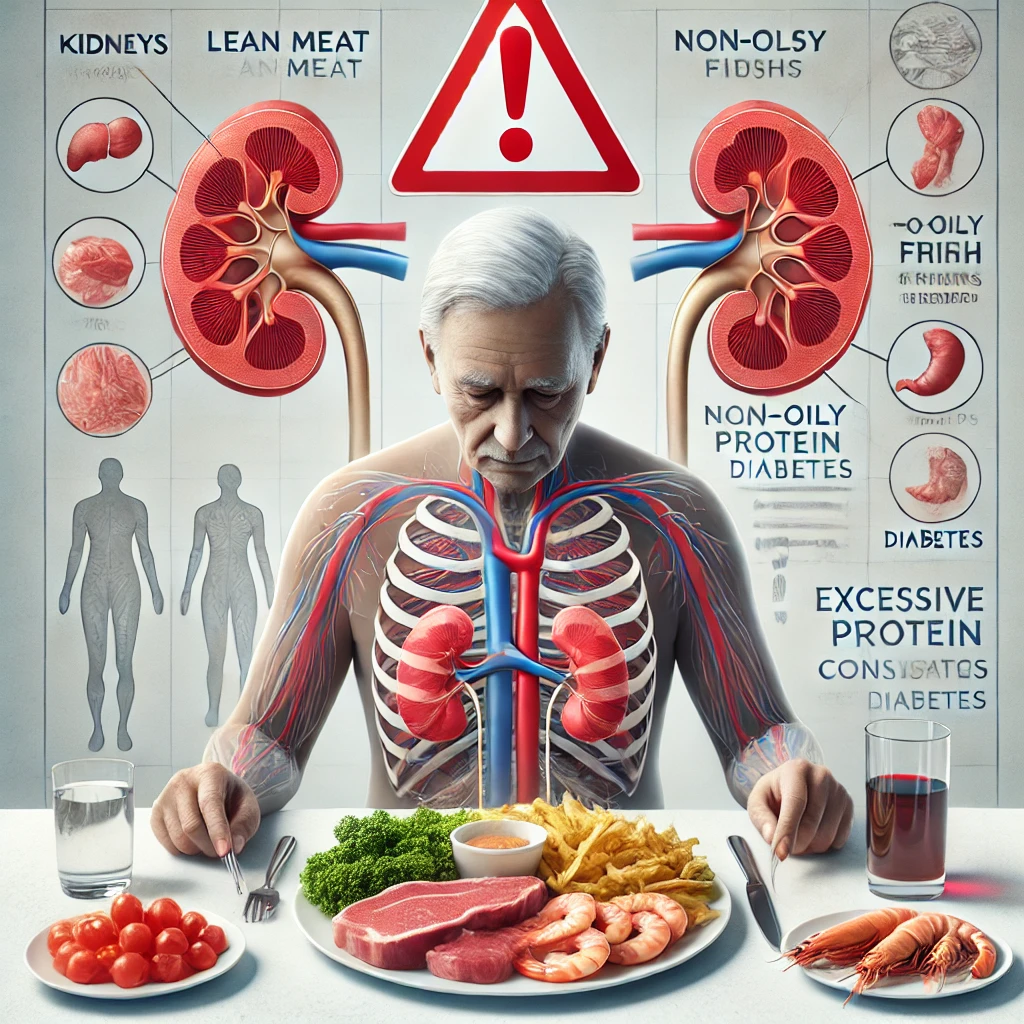
A prevalent misconception is that a high-protein diet is the primary culprit behind foamy urine. While it’s true that proteins can cause foam when they appear in the urine, the key factor is not the amount of protein consumed, but rather the kidney’s ability to filter and retain these proteins. In a healthy individual, dietary proteins are efficiently processed and utilized by the body. However, in diabetic patients, prolonged high blood sugar levels can damage the kidney’s filtering system, leading to protein leakage regardless of protein intake.
Balanced protein consumption remains a cornerstone of diabetes management. Modern dietary guidelines emphasize that patients should consume an adequate amount of protein to support bodily functions without overloading the kidneys. It is the compromised kidney function—rather than an excessive dietary protein intake—that is most commonly responsible for the appearance of foam in the urine. In essence, while protein is a necessary component of the diet, its presence in the urine often signals an underlying renal issue rather than simply reflecting dietary habits.
Beyond Protein: Other Organ Involvement
While proteinuria remains the primary and most direct cause of foamy urine in diabetic patients, it’s essential to recognize that our body systems work in concert. The liver, for example, plays a pivotal role in overall metabolism—it processes toxins, produces vital proteins, and regulates energy storage and usage. However, liver dysfunction does not typically cause protein to leak into the urine.
In diabetic patients, metabolic imbalances can affect multiple organs simultaneously. Although the liver may be compromised in conditions such as nonalcoholic fatty liver disease (NAFLD), these liver-related issues are usually distinct from the mechanisms that lead to foamy urine. Instead, the foam is predominantly a marker of kidney stress and damage, particularly due to the filtration challenges posed by diabetic nephropathy.
A holistic view of diabetes management acknowledges the interplay between various organ systems. Effective monitoring and management involve not just the kidneys, but also the liver, cardiovascular system, and overall metabolic health. This comprehensive approach allows for early intervention and can significantly mitigate the progression of complications, emphasizing the importance of proactive and integrative care.
Diagnosis and Medical Management
Effective diagnosis is essential for managing foamy urine, particularly in diabetic patients where it may signal kidney complications. Physicians typically begin with a detailed patient history and physical examination, followed by urine tests to detect protein levels. A simple urine dipstick test is often used as an initial screening tool for proteinuria. In some cases, a more detailed 24-hour urine collection may be recommended to accurately measure the amount of protein excreted.
If proteinuria is confirmed, additional tests are conducted to assess overall kidney function. Blood tests that measure creatinine levels and the estimated glomerular filtration rate (eGFR) provide critical information about how well the kidneys are filtering waste. Imaging studies, such as renal ultrasounds, can further help in evaluating kidney structure and detecting any abnormalities.
Early detection of kidney issues is paramount, as it opens the door to timely intervention. Management strategies generally focus on controlling blood sugar and blood pressure—key factors that influence kidney health. Medications like ACE inhibitors or ARBs are commonly prescribed, as they help reduce proteinuria and protect renal function in diabetic patients.
Furthermore, emerging diagnostic technologies, including advanced imaging techniques and biomarker assays, are improving early detection and allowing for more personalized treatment approaches. Regular monitoring and proactive management are crucial in preventing the progression of diabetic nephropathy and maintaining overall kidney health.
Forward-Thinking Approaches and Future Perspectives
The evolving landscape of medical research is providing promising avenues for the management of diabetic complications, particularly those affecting the kidneys. Emerging technologies and innovative approaches are shaping a future where early detection and personalized care can substantially alter the progression of diabetic nephropathy.
- Personalized Medicine and Biomarker Discovery:
Advances in genomics and proteomics are paving the way for identifying unique biomarkers that can predict kidney damage before significant proteinuria occurs. This personalized approach enables tailored treatment strategies that can more effectively slow down or prevent the progression of renal complications. - Integrative Therapies and Lifestyle Innovations:
Beyond traditional pharmaceuticals, integrative therapies are gaining traction. Combining dietary modifications, optimized physical activity routines, and stress management techniques with conventional treatments may provide a more holistic approach to managing diabetes-related kidney issues. Wearable technology and mobile health applications are also contributing to more continuous monitoring, empowering patients to make real-time adjustments to their lifestyle and treatment plans. - Technological Advancements in Diagnostics:
Cutting-edge imaging techniques and artificial intelligence-driven diagnostic tools are set to revolutionize early detection. By analyzing complex datasets, these tools can identify subtle changes in kidney function earlier than conventional methods, enabling proactive interventions that could significantly delay or even reverse early-stage kidney damage.
This forward-thinking perspective underscores a paradigm shift in diabetes management—from reactive treatment to proactive, precision care. As research continues to unveil new insights, patients and healthcare providers alike are better equipped to confront the challenges of diabetic nephropathy, ensuring improved outcomes and a higher quality of life.
Conclusion
Foamy urine in diabetic patients serves as a crucial early indicator of kidney complications rather than a mere consequence of a high-protein diet. The primary culprit—diabetic nephropathy—results from prolonged high blood sugar levels that compromise kidney function, leading to protein leakage into the urine. Recognizing this symptom early enables timely intervention, which is vital for mitigating further renal damage.
A proactive approach that combines regular monitoring, blood sugar management, and lifestyle modifications is essential for preserving kidney health. Additionally, the integration of innovative diagnostic technologies and personalized treatment strategies promises a future where diabetic complications can be managed more effectively and even prevented. Ultimately, understanding the underlying causes of foamy urine empowers patients and healthcare providers to adopt a comprehensive, forward-thinking strategy for long-term health and improved quality of life.